Why Funding For Paramedic Students Should Be Available To All
 By Megan Durling
By Megan Durling
As a student paramedic in England with a previous undergraduate degree, my motivation to become a paramedic comes at a significant personal cost — £27,750 in tuition fees to be precise.
Unlike my peers who are studying nursing, midwifery and nine other Allied Healthcare Professional (AHP) courses as a second undergraduate degree, paramedic students are prohibited from accessing any financial support from Student Finance England (SFE).
Of course, this was all news to me when I started my Paramedic Science degree at St George’s University of London in September 2018.
Two years earlier, I’d graduated from the University of Bath with a 2:1 Hons in BSc Natural Sciences and then worked as a mental healthcare assistant while deciding which medical career I wanted to pursue.
When I applied to study Paramedic Science I was told by Student Finance England that I would be entitled to funding for my degree because it was an AHP course.
But once I was accepted onto the course it later transpired that I would not be eligible for financial support afterall, which came as a huge shock.
The Impact On Students
It is estimated that five per cent of current students are affected by the lack of equity of funding, and for many prospective mature students this is a significant barrier to higher education.
In an attempt to overcome the financial implications of not being eligible for funding, many students look to paid employment alongside their education, which in itself can present numerous challenges.
For those who do find employment, trying to balance work, life, placement, study and possibly childcare can often result in students suffering from high levels of stress, anxiety, and ultimately burnout. Financial support could significantly ease some of this pressure.
In my case, I turned to my family for help. In an effort to contribute towards my tuition fees, my parents made the difficult decision to remortgage their home, to borrow additional funds, and my mother also chose to return to work in order to support me — a privilege I know not all students have, and one I am extremely grateful for.
But even with my parents’ contribution, it was still necessary for me to secure a part-time job working in a supermarket in order to sustain a living and pay for additional costs such as course equipment, and travel both to and from university, and to and from the locations of my placements across London.
These are just some of the considerations a mature student has to think about before pursuing a new career. Questions such as: Can I afford to live without a steady income? Will I be able to pay the rent? Can I afford childcare and the necessary travel costs to attend lectures and placement?
If they were studying nursing, midwifery or another eligible AHP course, then the answer to all of these questions would unequivocally be ‘yes’ because they would be entitled to receive full financial support. So why is it different if you want to become a paramedic?
Background
In 2017, the NHS Bursary Reform stated that those students beginning a nursing, midwifery or pre-registration AHP course would be eligible for full funding from Student Finance England, regardless if they already held an equivalent or lower qualification (ELQ).
Despite sufficient evidence to support Paramedic Science being a pre-registration AHP course, the same eligibility for funding rules, however, did not apply to paramedics.
Around the same time, the Health and Care Professions Council announced that as of September 1, 2021, the threshold for entry to register with them as a paramedic had been raised to Bachelor Degree with Honours in Paramedic Science.
While this was undoubtedly a great triumph for the paramedic profession, it made the vast disparity in accessing funds glaringly obvious.
How could student paramedics, who now hold the same professional level qualification as their Allied Health Profession peers, continue to be denied funding when financial assistance is so readily available to those studying other AHP courses as a second degree?
I’m sure most people would agree that we have played, and continue to play an equally vital role as that of our AHP counterparts in the provision of health and care in this country.
The Learning Support Fund
In January 2020, the Department of Health and Social Care announced all new and existing paramedic students studying at English universities would benefit from additional NHS funding in the form of the Learning Support Fund (LSF) to support the financial implications of their training.
In real terms, this meant that a £5,000 grant was available and student paramedics were at last being offered a much-needed financial lifeline.
However, delight quickly turned to frustration when it emerged that those students who held a previous degree would not be eligible for the LSF.
In order to be entitled to the grant, students must qualify for funding from Student Finance England which begs the question: Why is the grant only offered to those already in receipt of financial support?
Final Thoughts
As a paramedic student with a previous degree, all I am asking for is a level playing field with my AHP peers, with whom we work in tandem to provide care and support to our patients across the UK.
I believe that to accomplish this, all paramedic students, as deserving members of the Allied Health Professions, studying either a primary or secondary degree, should be eligible for financial support throughout their studies, from Student Finance England and the Learning Support Fund to cover tuition fee costs and associated living and travel expenses.
For me, choosing to become a paramedic is the best decision I’ve ever made, but without my family’s support I know it wouldn’t have been possible.
I’m one of the lucky ones, but there are countless students with undergraduate degrees who would dearly love to become paramedics and can’t, simply because there’s no financial aid available to them. It’s so unjust, and we need it to change.
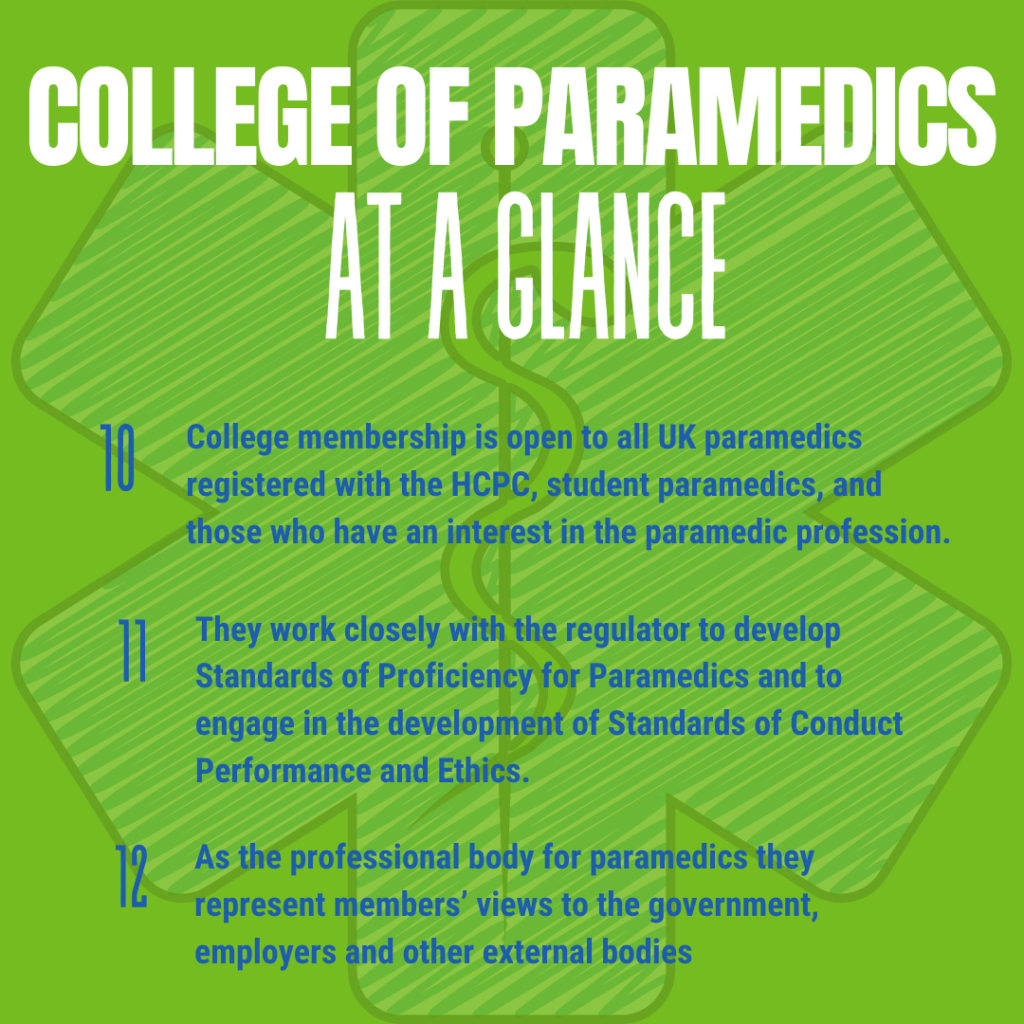
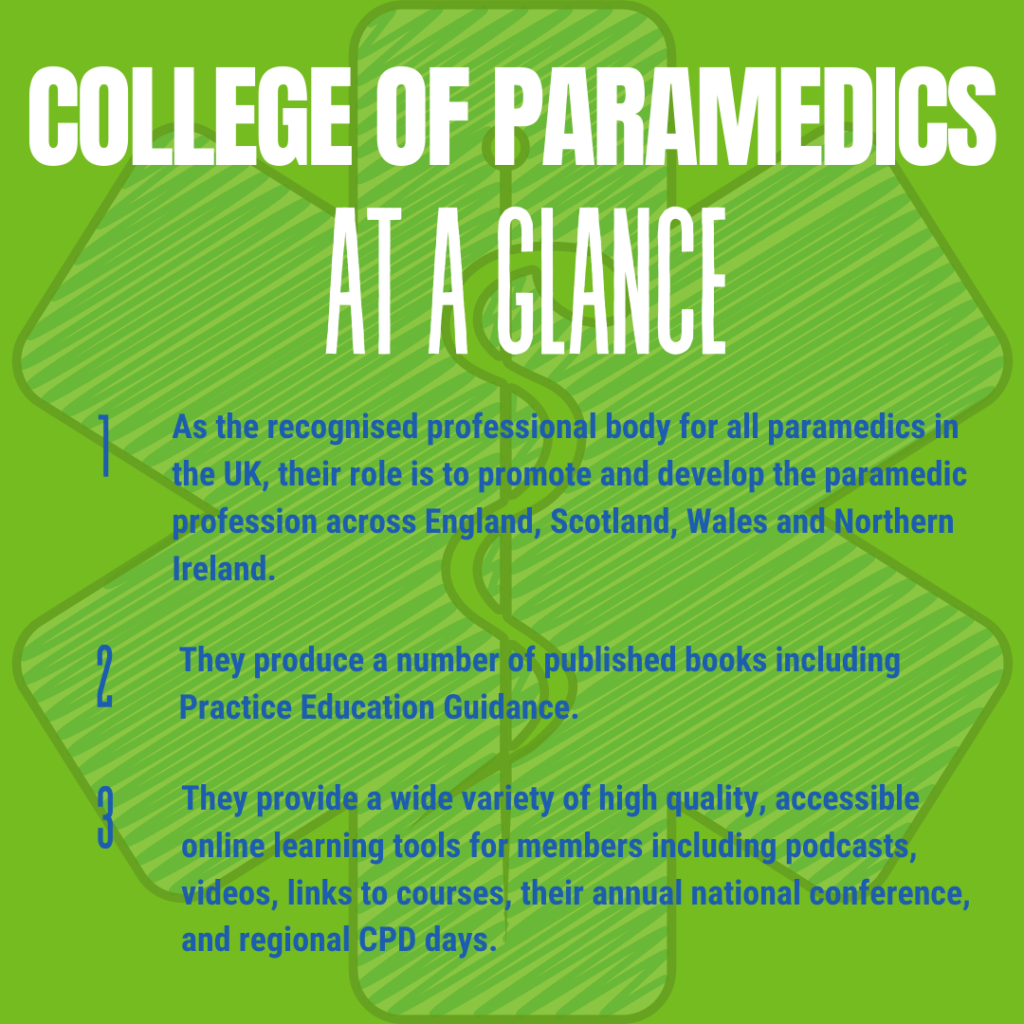
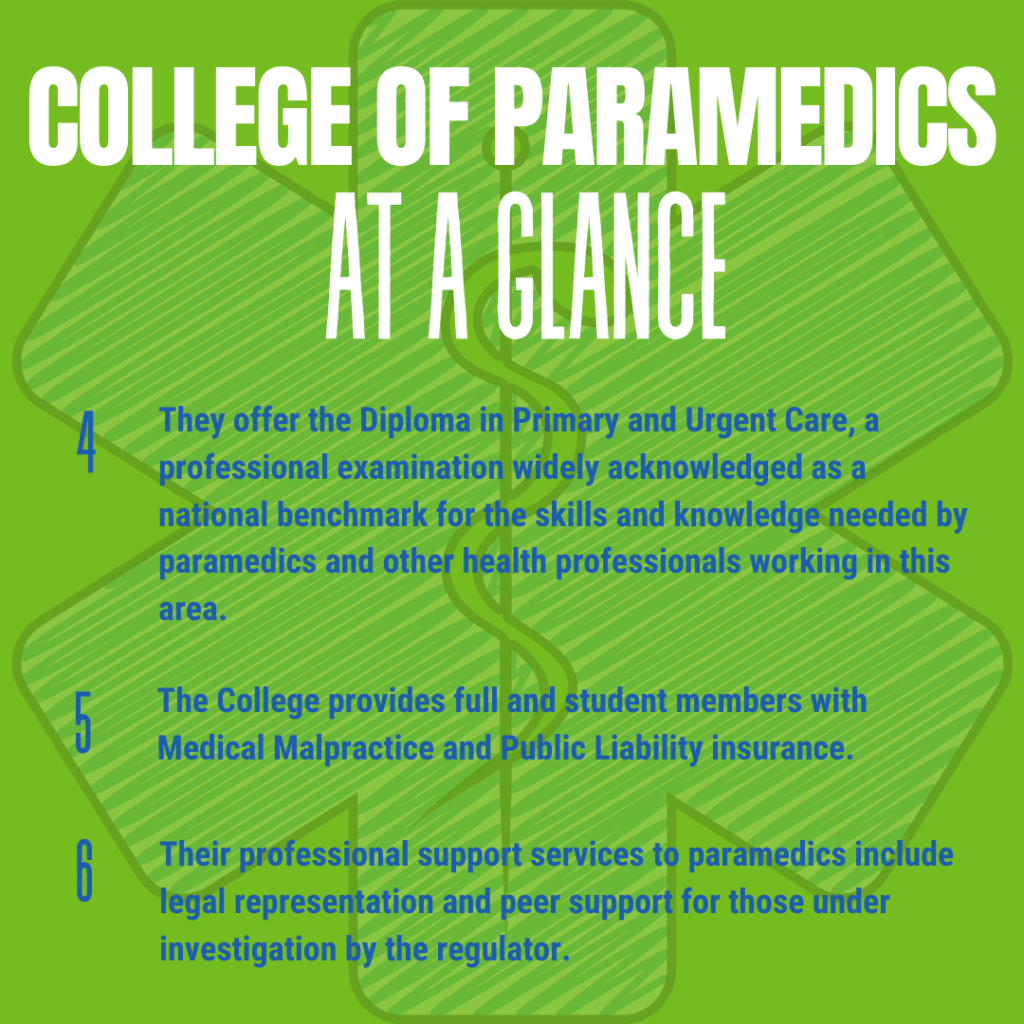
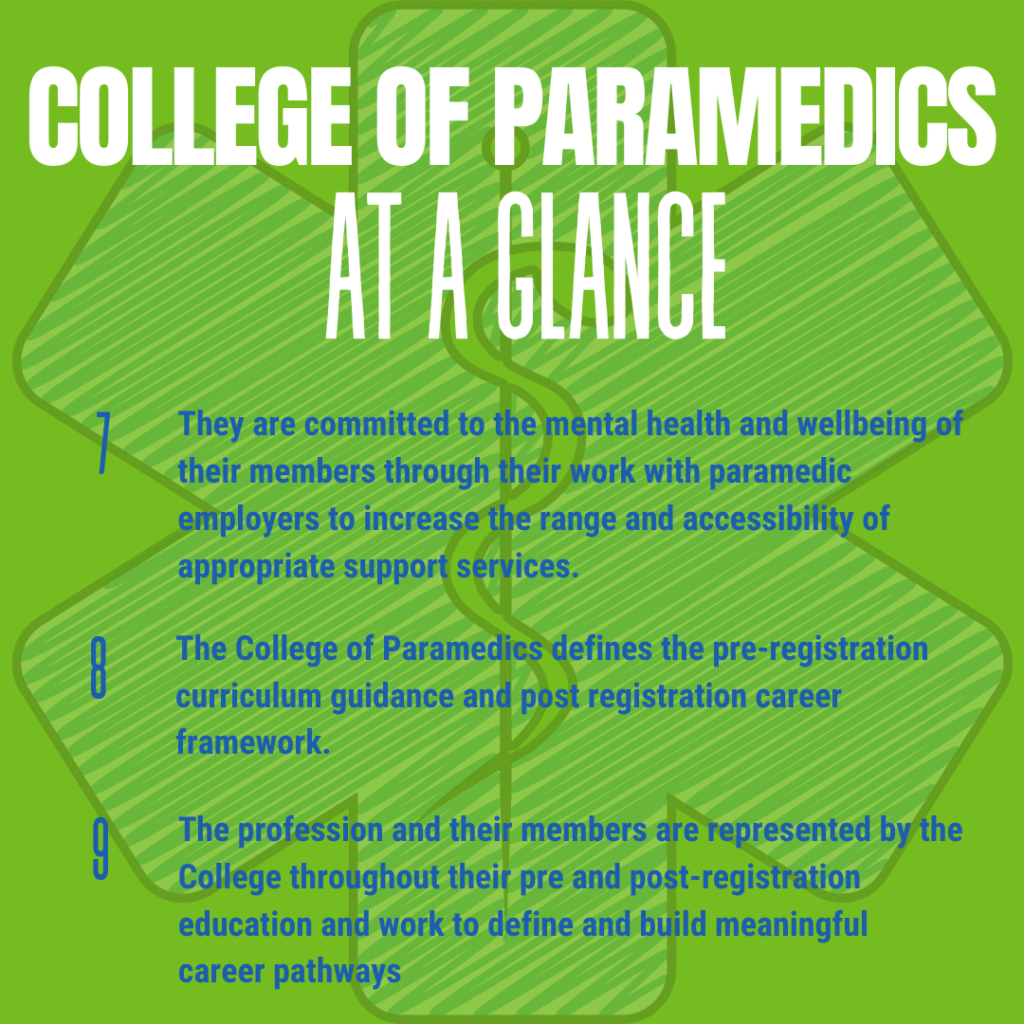
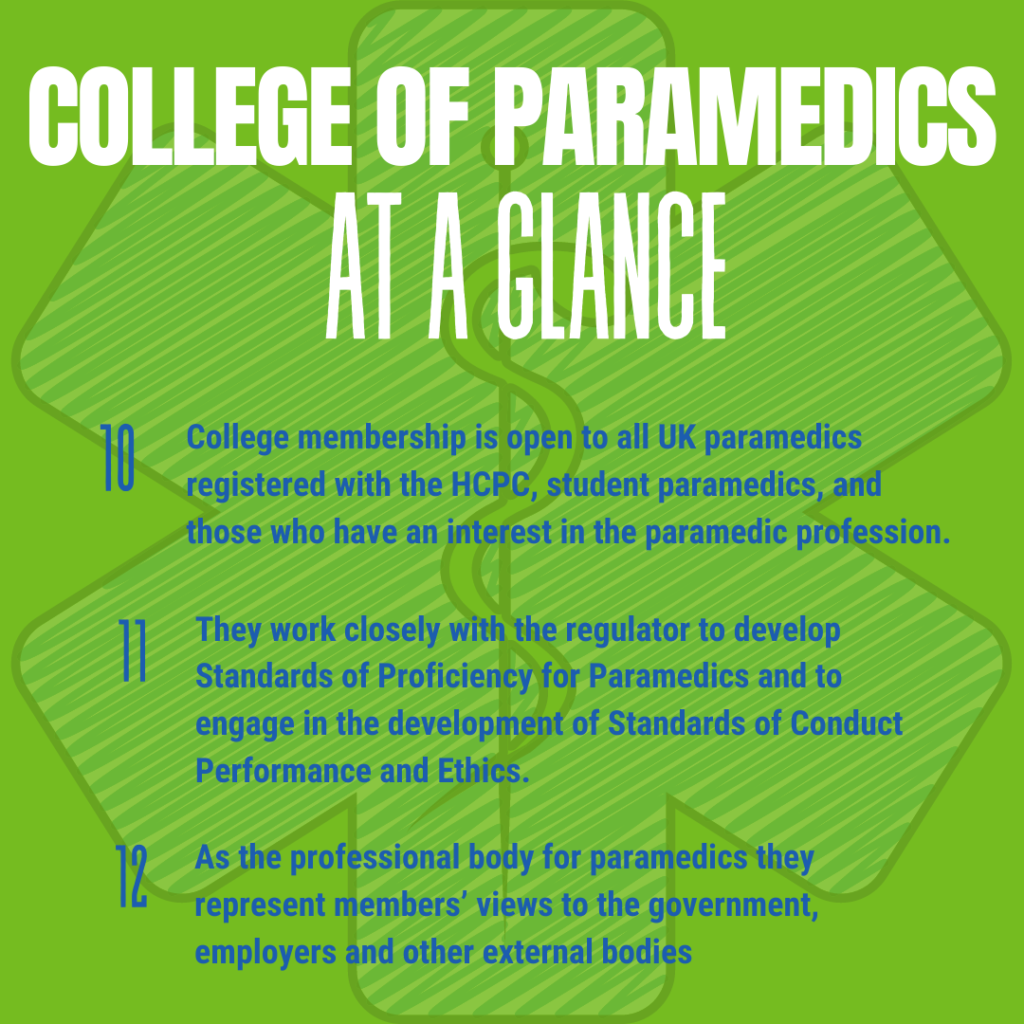
For more information and to support the campaign, visit www.collegeofparamedics.co.uk - News - Campaign for Student Funding.
For enquires please contact the campaign’s Student Press and Communications Officer, Charlotte Austwick: [email protected]
Or Student Campaign Manager, and author of this piece, Megan Durling: [email protected]
Quality content
- Casinos Not On Gamstop
- Casinos Not On Gamstop
- Casino Sites Not On Gamstop
- Non Gamstop Casino
- UK Online Casinos Not On Gamstop
- Casino Sites Not On Gamstop UK
- Casino Sites Not On Gamstop
- Games Not On Gamstop
- Sites Not On Gamstop
- UK Online Casinos Not On Gamstop
- Casino Not On Gamstop
- Slots Not On Gamstop
- Casino Not On Gamstop
- Gambling Not On Gamstop
- Casinos Not On Gamstop
- Non Gamstop Casino
- UK Online Casinos Not On Gamstop
- Casino Sites Not On Gamstop
- Best Betting Sites
- Best UK Online Casinos
- New Horse Racing Betting Sites